The Delta variant explained—and why it’s so important

Just when you’ve loosened up on wearing a mask in public, or perhaps felt a rush of gratitude for being able to go about life, travel and family visits more freely, here comes the “Delta variant,” a genetic mutation of coronavirus that is contributing to a surge in COVID-19 cases in the United States and around the world.
While several variants have been identified (Delta, Alpha, Gamma, Beta)—and there will be more mutations to come—the Delta variant is spreading the most quickly.
Thankfully, science and medicine are keeping up with the virus. As of August 23, 2021, the FDA has approved the COVID-19 vaccine made by Pfizer for BioNTech. Previously, this vaccine was authorized for emergency use only. It has proven to meet the FDA’s rigorous standards for safety and effectiveness in preventing COVID-19 spread and illness, and it is now FDA-approved as a two-dose series in people 16 years and older. It is also authorized for emergency use and COVID prevention, to be given to youth ages 12 to 15 years old, and as a third dose given to people 12 years of age and older with certain immunocompromised conditions.

Here’s what we know about the Delta variant:
- One person can infect about five others—more than twice the original variant. That means that more people are getting more infected more quickly. And the more the Delta variant circulates, the more it mutates. The more mutations, the greater chance of becoming a variant that is resistant to vaccination.
- A vaccinated person can still get infected with the Delta variant. These are called “breakthrough” cases, and we will continue seeing them as more and more people get vaccinated. This doesn’t mean the vaccines don’t work—breakthrough cases are just more likely to occur as vaccinations increase.
“Keep in mind that being infected doesn’t mean you’ll get sick or die,” says Lawrence Livornese, Jr, MD, an infectious disease specialist at Main Line Health. “Being infected with the Delta variant without being vaccinated, however, does put you at greater risk for sickness, hospitalization and death.”

- A vaccinated person infected with Delta can transmit the virus just as much as an unvaccinated person. This means that even if you’ve been fully vaccinated, there is high risk of transmission if you’ve have been infected with the Delta variant. So you should continue wearing a mask wherever there’s a strong possibility of transmission, such as in large groups of people or areas where a lot of people pass through. You should also mask up in geographic “hot spots” and higher transmission areas.
- An unvaccinated person who gets sick with the Delta variant is more likely to have more severe symptoms. While getting vaccinated for COVID-19 does not completely prevent infection, it can help minimize how severely ill you get if you become infected with the Delta variant.
The more the Delta variant circulates, the more it mutates. The more mutations, the greater chance it has of becoming a variant that is resistant to vaccination.
Why should I bother getting vaccinated if there will always be more mutations?
You may find it hard to see the logic of getting vaccinated against one strain when new strains just keep on appearing. And, of course, there will always be risks associated with any disease prevention measure, just as there are risks with any cure. The question is whether the benefits outweigh the risks.
For the most part, vaccines save lives and minimize sickness in most people. Your response to a vaccine is based on a number of factors, including your age, health status, genetics and unique aspects of your own immune system—even social and cultural influences. But COVID vaccines have been undeniably proven to:
- Control rapid spreading of coronavirus
- Minimize spread of Delta variant
- Reduce severity of symptoms in infected people
Vaccines have protected millions of kids around the globe against serious childhood illnesses. There are many diseases we hardly hear of anymore because vaccination works so well—polio, rubella and measles, to name a few. According to infectious disease specialist Livornese, “Most vaccinations for children are more than 90% effective at disease prevention. If a child who has been vaccinated does get the disease, they usually have far fewer symptoms or complications. An unvaccinated child, on the other hand, is more likely to be infected and have worse symptoms.”
While vaccines remain “imperfect” (always carry risk), they result in a tremendous reduction in symptoms, spread and severity—as well as huge payoffs in the health of people and the economy.
So while vaccines remain “imperfect” (always carry risk), they result in a tremendous reduction in symptoms, spread and severity—as well as huge payoffs in the health of people and the economy.

How much am I really at risk for COVID or the Delta variant?
Keep in mind that “risk” involves more than just personal risk. Risk can refer to:
- Contracting COVID yourself
- Spreading COVID to your community
- Infecting vulnerable friends and family members
If you’re not vaccine-eligible, you’re at even greater risk of contraction and complications. People who aren’t eligible for COVID vaccination include children 12 years old and under, certain people with compromised immune systems, and people with various types of allergies.
Not getting vaccinated is not an option anymore. Everyone who is eligible to receive COVID vaccination needs to get vaccinated so we can slow the spread and the suffering caused by this disease. – Dr. Lawrence Livornese, Infectious Disease Specialist and Chair of the Department of Medicine for Main Line Health
Young people and adults with underlying conditions remain particularly vulnerable. Common underlying conditions include:
- Asthma and respiratory diseases
- Diabetes
- Heart disease
- Influenza (flu) and pneumonia
- Obesity
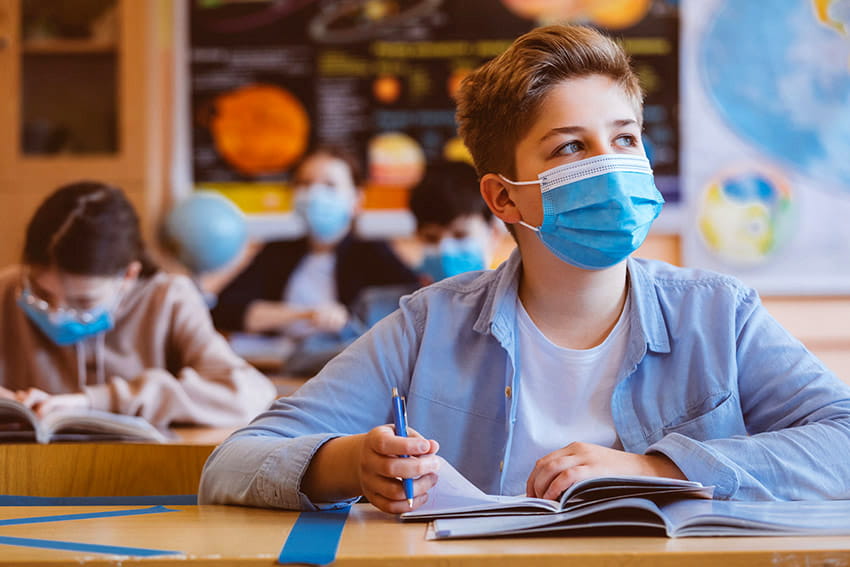
More than four million children in the United States have tested positive for coronavirus.[1] Infections among children are on the rise, mostly because of the Delta variant. Children may have fewer symptoms or complications from the disease, but they’re still vulnerable to long-term, lasting effects (long-haul COVID), and they can easily spread the virus to others.
With the rise of the Delta variant, we are all vulnerable to infection, whether we show symptoms or are asymptomatic—never have any symptoms at all. Regardless of age, race, gender, socioeconomic or immunization status, we’re all capable of transmitting coronavirus to others and having it transmitted to us. “We’re all at risk—and we put everyone else at risk, often unknowingly and unintentionally,” as Livornese points out.
“Not getting vaccinated is really not an option anymore. Everyone who is eligible to receive COVID vaccination needs to get vaccinated so we can slow the spread and the suffering caused by this disease. While this is a unique and highly personal decision, I feel strongly that we have an obligation to get vaccinated and protect those that can’t receive the vaccine or may not respond as well to the vaccine, such as our children, the elderly and cancer patients.”
Vaccination is still the best possible way to minimize spread, infection, illness and death, according to the medical and scientific community.
The American Academy of Pediatrics recommends that all eligible young people ages 12 and older be vaccinated to prevent against COVID-19.
Whom should I trust about COVID vaccination?
Your decision to vaccinate yourself or your family is entirely up to you, of course. Just be sure to weigh your own best judgment and common sense with accurate, up-to-date medical and scientific sources. Don’t rely on hearsay and opinions, or examples of individual cases or experiences.
Medical and public health experts—people whose lifework is to protect the health of the public—put vaccines through a tremendous amount of scrutiny. Representatives from dozens of organizations come together to assess the effectiveness and safety of vaccines, and to adjust course based on feedback and results.
Although vaccines to protect against coronavirus didn’t previously exist, the exact “technology” needed to develop COVID vaccines did exist. Explains Livornese, “We had successfully used this vaccine technology for other types of diseases. That’s why the Moderna and Pfizer vaccines were approved for emergency use so quickly.”
‘Herd immunity’ and why you shouldn’t wait it out
You may have heard about the idea of “herd immunity.” In this scenario, a lot of people are vaccinated, and some are not. The idea is that when enough people have become immune to infection, it’s less likely that people who aren’t immune—who haven’t been vaccinated—will get infected.
When we first started hearing about how many Americans would need to be vaccinated, the numbers were about 60 to 70 percent vs. the rest of the (unvaccinated) population. Meaning, more than 60 percent of us would need vaccination to achieve herd immunity.

Well, 60 percent of Americans have received at least one dose, and about half of us are fully vaccinated. But now the Delta variant is driving the need for more like 80 to 90 percent immunization rates, in order to limit mutation and the debilitating effects of the virus.
Herd immunity comes at a cost. During the 1918 flu pandemic, tens of millions of people died before human immune systems had a chance to adapt and fight off the virus.
When will it end?
Will it ever end?
Will we have to keep waiting for new, better vaccines while still standing by as people get sick and die?
Or will there be more and more infections by different strains of virus that we can’t possibly control?
The challenge of new virus strains requires us to continue thinking in terms of the greater good vs. just about ourselves.
These are all valid questions and concerns. And yes, the situation is extremely difficult—for everyone. Disease experts, health care providers, mental health practitioners, parents and caregivers around the globe all feel the frustration.
All we can do now is accept that this is where we are, locally, nationally and globally. Adds Livornese, “The coronavirus and the challenge of new virus strains require us to think in terms of the greater good vs. just about ourselves, and to operate in unity for the sake of our families, jobs, schools, communities and economy.”
Find out more about COVID vaccines or register today for vaccination.
Main Line Health serves patients at hospitals and health centers throughout the western suburbs of Philadelphia. Find out more about vaccine availability and scheduling at Main Line Health.
[1] American Academy of Pediatrics and Children’s Hospital Association
 Content you want, delivered to your inbox
Content you want, delivered to your inbox
Want to get the latest health and wellness articles delivered right to your inbox?
Subscribe to the Well Ahead Newsletter.
