Surviving the emotional impact of birth trauma, and helping others do the same: Kayleigh’s story
The last thing Kayleigh Summers remembers from that chapter in time is getting her nails done on a Friday afternoon. At age 29, the former Division I soccer player was 40 weeks along and enjoying a perfectly healthy pregnancy. But the following Monday, her entire world would turn upside down.
The understanding she now has of what transpired over the next 10 days would come through accounts shared by her loved ones and members of her extraordinary medical team, and by scouring 6,000 pages of her own medical records.
On July 15, 2019, Kayleigh attended her regularly scheduled appointment at the Collegeville office of Main Line OB/GYN. A high blood pressure reading prompted a directive to visit the Labor and Delivery Unit at Paoli Hospital, part of Main Line Health, as a precaution, where the decision was made to induce her. It took two full days ― until that Wednesday at noon ― for Kayleigh to become fully dilated. Although this timeframe is not abnormal, she was feeling unusually anxious.
When Kayleigh's OB/GYN, Mojdeh Saberin, MD, confirmed it was time, Kayleigh's mom, who was planning to stay in the room during delivery, headed out to the waiting room to let Kayleigh's dad know the baby was coming. Kayleigh's husband Steve remained by her side.
It was in that exact moment Kayleigh knew something was terribly amiss. She began screaming that something was wrong with her heart. She would later learn there is a medical term for this feeling. It is known as a "sense of impending doom" ― an intense feeling that something threatening or tragic is about to occur, despite any apparent danger.
Seconds later, Kayleigh experienced full cardiac arrest.
Code Blue: Fast action to save Kayleigh and her baby
Kayleigh's nurse hit the code blue button, and the medical team at Paoli Hospital sprang into action, rushing Kayleigh into the operating room (OR). Dr. Saberin realized right away Kayleigh was experiencing an amniotic fluid embolism (AFE) ― a rare and life-threatening complication that occurs when amniotic fluid gets into the bloodstream and causes an immune response just before, during or immediately after childbirth.
Within six minutes of the code, Dr. Saberin delivered baby Callahan (Cal for short) via cesarean section. The medical team in the OR, which included several OB/GYNs and three cardiac specialists who ran in when the code was called, was still performing cardiopulmonary resuscitation (CPR) on Kayleigh. It took ten minutes of chest compressions to bring her back.
Once Kayleigh's heart rate was established, anesthesiologist Archie Sirianni, MD, rapidly intubated her and administered the appropriate course of medications. It would be only the beginning of her journey.
As is common with AFEs, Kayleigh experienced disseminated intravascular coagulation (DIC) ― a serious blood clotting disorder that leads to uncontrollable bleeding and prevents blood and oxygen from flowing to the head, heart and other organs. Dr. Saberin had anticipated this distressing complication, inserting a fluid-filled balloon in Kayleigh's uterus to compress the vessels that were bleeding. And she quickly ordered a massive transfusion protocol. Dr. Sirianni added vasopressors to Kayleigh's medications, which place pressure on the blood vessels to squeeze oxygen-rich blood back into the vital organs.
But Kayleigh continued to hemorrhage.
For the next five hours, an ever-expanding team of experts at Paoli Hospital, led by the primary trauma surgeon, would work together at a frenetic pace to save Kayleigh's life.
Saving Kayleigh
Kayleigh was unable to breathe on her own. So, immediately the Paoli Hospital team reached out to their cardiac colleagues at Lankenau Medical Center, who have a team of experts trained in extracorporeal membrane oxygenation (ECMO). ECMO is a condensed heart-lung machine that temporarily supports the heart and lungs when one or both are not functioning due to disease or trauma. Both the ECMO and the team of experts were swiftly transported to Paoli Hospital.
As Kayleigh was placed on ECMO, she experienced a second cardiac arrest ― two hours after the first code was called ― and would be brought back to life again.
The relentless bleeding from Kayleigh's uterus continued to fill her abdomen. Paoli Hospital's interventional radiology team performed a uterine artery embolization ― a procedure where a catheter is used to deliver small particles that block the blood supply to the uterine body. But it would not be enough. The only way to stop the bleeding was for the medical team to perform a hysterectomy and remove Kayleigh's uterus, as well as one of her ovaries.
Kayleigh would require more than an astonishing 140 units of blood as her team fought to control the DIC. Her surgical team then packed her abdomen with gauze and left the incision open, as they knew they would need to go back in several more times to assess and address any additional bleeding.
All the while, Dr. Saberin was running in and out of the OR to the waiting room, and soon to a dedicated conference room just down the hall, to communicate with the growing number of Kayleigh's family and friends who were gathering. The hospital chaplain remained steadily by her father's side.
"When I first went to tell Kayleigh's family about the AFE, I cried in the hallway," says Dr. Saberin. "50% of women with AFEs aren't alive after 10 minutes. Kayleigh came into the hospital to have a baby. You don't predict dying when you're going to have a baby."
Providing exceptional care

When baby Cal arrived at Lankenau Medical Center, the nurses placed him on Kayleigh's chest for skin-to-skin contact, which is scientifically proven to help both moms and babies. The nurses continued to do so at least once a day while Kayleigh remained on ECMO, fighting to come back.
Mara Caroline, MD, an interventional cardiologist specializing in critical care cardiology and mechanical circulatory support, would need to implant an Impella ― the smallest heart pump in the world ― to allow Kayleigh's heart time to recover. There would be three more abdominal surgeries over the next several days to address damage caused by the DIC.
By Friday, Kayleigh's heart and lungs were improving. The Impella was removed, and she was taken off ECMO. Saturday night, her breathing tube was removed.
"Kayleigh's recovery was shockingly miraculous," says Dr. Saberin. "She was in the right place at the right time with the right people there. The coming together of all the different specialties ― the blood bank, trauma surgery, OB/GYN, interventional cardiology, interventional radiology, the nursing staff, even the medical students who held the OR door open as everyone ran in and out ― all of these specialties seamlessly came together, and that is what saved her. And the leadership of Dr. Joseph Gobern, system chair of Obstetrics and Gynecology at Main Line Health, who sets the highest of standards for us. What we were able to do for Kayleigh is at the cutting edge of what medicine today is capable of."
Facing the future
"The first thing I remember is the next Monday morning, when Dr. Saberin and Dr. Sirianni came to Lankenau Medical Center," recalls Kayleigh. "They sat at each side of my bed, holding my hands, and they told me what happened. They told me it was a miracle I was alive. And they told me I wouldn't be able to have more children. They had offered that to my family, who didn't know how to tell me."

Fourteen days after experiencing a devastating AFE, Kayleigh was able to go home, where the next chapter in her long road to recovery would begin. Visiting nurses came daily to pack her incision. Her parents moved in to help with Cal.
"It was tough," shares Kayleigh. "I was sleeping 16 hours a day. I couldn't take care of my baby at all. It was hard that all of his firsts were happening without me. But I was bone tired. My body was completely ravaged."
It would take another 18 months for Kayleigh's body to heal, including undergoing another surgery to repair a massive hernia and completely reconstruct her abdomen. She was insistent that Dr. Sirianni serve as the anesthesiologist, and that her trauma surgeon perform the procedure. She trusted them completely and had grown very close to them, as well as other members of her medical team. They had all gone through so much together.
Healing emotionally was something entirely different.
"I know how incredibly lucky I was," says Kayleigh. "I know my doctors were amazed that I survived, and that I did so without any lingering issues was crazy. They were elated. But all I could think of at that time was that my uterus was gone, I wasn't present for my baby's birth and I couldn't even act like a mom. I was so grateful, but I also felt so angry and sad."
Coping with birth trauma
"Six months after Cal was born, I had this moment of, 'Why isn't anyone out there talking about this,'" says Kayleigh. "I was seeing all of these birth announcements, classes about birthing and parenting, and the whole social aspect of it. And no one was talking about birth trauma. No one was talking about the magnitude of how many lives are affected. I kept thinking, 'How can I use my skillset to do something? What can I offer?'"
At the time, Kayleigh and Steve had been working together at a boarding school ― Kayleigh as a therapist. It was January of 2020 when she decided to start an Instagram account to share her story, with the hope of creating a supportive community for others who had experienced AFE and other types of birth trauma. Her following quickly expanded to 1,000, and she added TikTok to her channels. Then her story went viral. And her social presence grew exponentially.
"I knew the feeling I was having wasn't unique to me," she says. "Every AFE survivor I've ever spoken to shared similar feelings. I knew I survived something I shouldn't have, and I needed to honor all the moms who didn't make it out, and try to help those who did."
Paying it forward
Kayleigh remained in her position at the boarding school while her social presence continued to amplify. She opted to participate in additional training to hone her expertise in perinatal mental health, trauma therapy and other specialty areas. In July 2022, she opened a private practice where she offers both individual and couples therapy to those who have experienced birth trauma.
In addition to her private practice, she's widely known as the Birth Trauma Mama and highly regarded by her 161,000 Instagram followers (@thebirthtrauma_mama) and 412,000 followers on TikTok. She hosts a popular podcast with a five-star rating. And she works with the AFE Foundation, providing outreach and support to survivors and to grieving families. She's deeply committed to helping people put the pieces back together.
"I think we sometimes forget how valuable community is, how valuable shared experiences are in the healing process. When I post about my story through my own lens, I know I'm not hitting everyone's personal story, but others who comment have common stories, and they're all connecting with each other. That was always my goal," says Kayleigh. "On one side, it feels incredible to be able to take something so devastating and awful and use it to help others, to take some of the worst moments of my life and use it to help guide people to the other side, knowing for those who can't yet see it that there is another side, I'm holding that place for them. On the other side, I'd give all of this back in a heartbeat if I could have had a better experience with Cal's birth, or if I could have more children."
Life today
Now age 33, Kayleigh reports that life is great. She and Steve recently bought a home in Downingtown. They're very close with their extended family, and enjoy spending time together in Ocean City, New Jersey — where Kayleigh's parents have a house — and at their own home. Cal especially loves playing "construction site" in the yard.
Cal is the best," says his proud mom. "He has the most spirited personality. He's rough and tumble but also very sweet. He feels hard. He loves hard. He has big emotions."
Kayleigh credits her amazing support system for helping her through the darkest times.
"There are a lot of things I've had in my corner," she says. "I have an incredibly supportive family who let me talk about what happened every day. I was crying for like a year. My family all came together on Cal's first birthday and made a champagne toast to celebrate that I survived. They're so good about honoring my experience. They're always leaving space for that. I know not everyone has that.
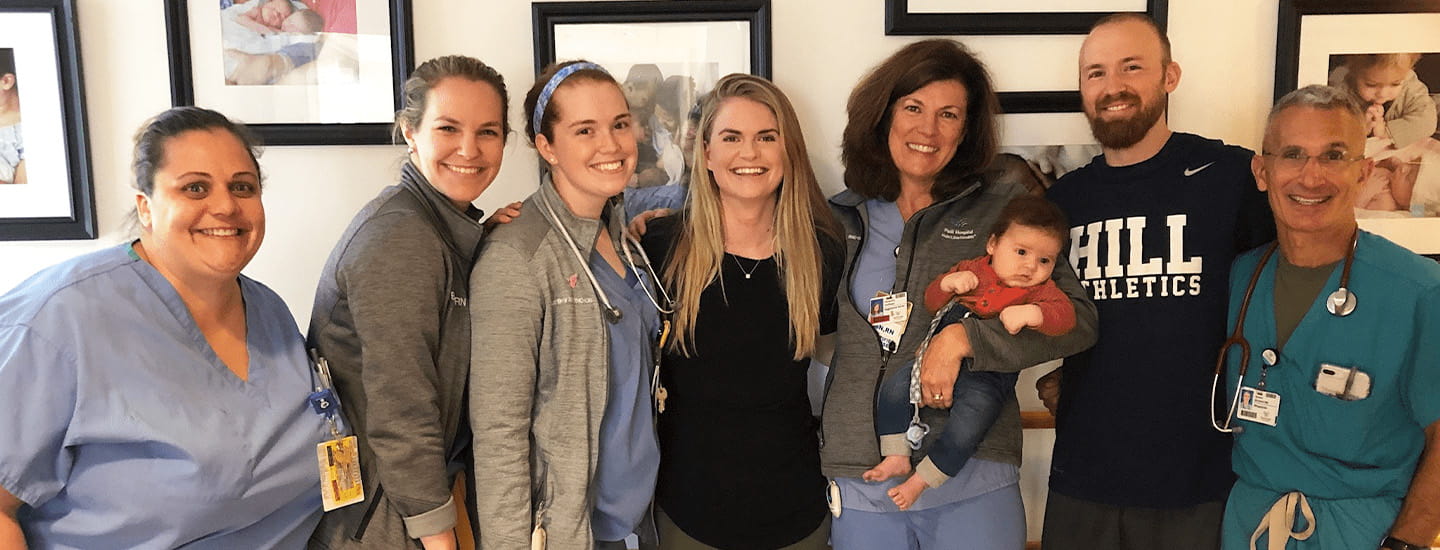
"Another big, massive piece is the way my care teams at Paoli Hospital and Lankenau Medical Center took care of me and my baby and my family, and how they continued to show up for me emotionally after I went home, checking in regularly. I had so much health anxiety after this happened, and I went through major depression. Their support changed the course of my recovery. They were always there. They still are. Two of my nurses and Dr. Saberin even come to Cal's birthday party every year."
Kayleigh knows she's right where she needs to be.
"I'm not a big 'everything happens for a reason person,''' she says. "I don't believe my AFE happened for a reason. That I survived the way I did, pretty much unscathed, I feel like there's reasoning behind that. What I'm doing now feels like exactly what I was meant to do, what I was put here to do, given the cards I was dealt. I know I got very lucky. I know there were a lot of things in my favor and a lot of incredible people around me. And I am so very grateful."
Next steps:
Learn more about Mojdeh Saberin, MD
Learn more about Kayleigh Summers, LCSW (The Birth Trauma Mama)
Learn more about obstetrics/gynecology and maternity care at Main Line Health
Want to get the latest health and wellness articles delivered right to your inbox?
Subscribe to the Well Ahead Newsletter.
 Content you want, delivered to your inbox
Content you want, delivered to your inbox
Want to get the latest health and wellness articles delivered right to your inbox?
Subscribe to the Well Ahead Newsletter.
