Can ancestry testing detect genetic heart disorders?

Heart disease is the leading cause of death for men, women, and many racial and ethnic groups. An estimated one in four deaths is attributed to heart disease. Many of the risk factors for heart disease are manageable; factors like smoking, obesity, alcohol intake, diet and a sedentary lifestyle. But one risk factor you can’t control is your genes.
Genetic factors play a role in determining cardiovascular disease risk. High cholesterol, arrhythmias, cardiomyopathy, aortic aneurysms and dissections and congenital heart disease are just a few of the chronic issues that can be passed down from generation to generation.
The more you know about your family’s heart health history, the better prepared you’ll be to manage your cardiovascular disease risk.
The value of ancestry tests in determining health risks
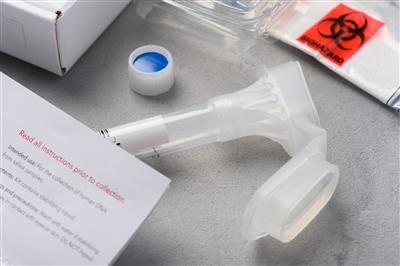
Over the past several years, companies like AncestryDNA and 23andMe have made DNA testing accessible to the masses. Their promise is simple: Submit a saliva sample via mail, and you’ll receive a comprehensive report of your genealogy—a chance to discover relatives, understand your family’s origin and ethnicity, and even get information that could help you make more informed decisions about your health.
Even though this information is helpful to have, it doesn’t have the same value as genetic counseling and testing. Genetic counseling is available at many hospitals across the country, including Main Line Health, and offers personalized clinical insight into the health risks that are unique to you, including discussion and coordination of clinical grade genetic testing, if appropriate.
“DNA analysis from ancestry testing companies may include health information related to the most common genetic variants associated with disease, but the analysis is not as thorough as a clinical grade test and therefore may give a false sense of security. Additionally a genetic variation found through an ancestry test may need to be confirmed with a clinical grade test,” explains Cristina Nixon, MS, LCGC, a licensed genetic counselor at Main Line Health.
What makes genetic testing different
If you want to better understand your risk for heart disease or hereditary cardiovascular disease, your best option is to talk to your health care provider about genetic testing. Unlike ancestry tests, genetic testing is done solely for the purposes of determining what health conditions you may be at greater risk for and steps that you can take to manage that risk.
While genetic testing is beneficial, it’s not necessary for everyone. Cardiovascular genetic testing likely won’t be recommended if you have a parent with high blood pressure or a grandparent that had a heart attack late in life, but your health care provider might recommend it if there is a history of unexplained cardiac events in your family.
“If someone in your family did not have the traditional risk factors for a cardiac death—smoking, diabetes, obesity, etc.—but suffered a heart attack or cardiac arrest, that is something that’s worth investigating,” explains Nixon. “It means that there could be an underlying genetic risk that you may not be aware of.”
You might also be a candidate for cardiovascular genetic testing if you have:
- A family history of aortic aneurysm, aortic dissection, cardiomyopathy or arrhythmia
- A family history of early heart attacks (Men: under age 55 years; women: under age 65 years)
- A congenital heart defect
- Untreated LDL cholesterol (higher than 190)
- Unexplained accidents, seizures or fainting
These are just a few of the factors that might make you a candidate for cardiovascular genetic testing. The best way to determine whether or not it’s right for you is to talk to your health care provider. If you pursue genetic evaluation and are found to have an inherited cardiovascular disease or be at a greater risk for cardiovascular disease, a genetic counselor will review and discuss your results with you and help you determine a path to manage your risk. This step, in particular, is what makes genetic testing a better option for assessing and understanding your cardiovascular risk.
"Deciding to pursue ancestry testing is a personal choice and can be interesting, but I urge anyone who has concerns about their cardiovascular risk factors to talk to their doctor about genetic counseling and how it can benefit them."
Additionally, an inherited cardiovascular disease may have implications for family members, which would also be discussed during your genetic counseling appointment.
“Ancestry testing does not offer you insight, explanation or guidance about your results in the way that genetic counseling and testing does. Deciding to pursue ancestry testing is a personal choice and can be interesting, but I urge anyone who has concerns about their cardiovascular risk factors to talk to their doctor about genetic counseling and how it can benefit them,” says Nixon.
Main Line Health’s Genetics and Risk Assessment Program offers genetic counseling and coordination of genetic testing for cardiovascular, cancer and prenatal genetics, as well as the opportunity to participate in genetic research. Learn more about our program online or call 484.565.GENE (4363) Monday–Friday, 8:00 am–4:00 pm.
 Content you want, delivered to your inbox
Content you want, delivered to your inbox
Want to get the latest health and wellness articles delivered right to your inbox?
Subscribe to the Well Ahead Newsletter.
