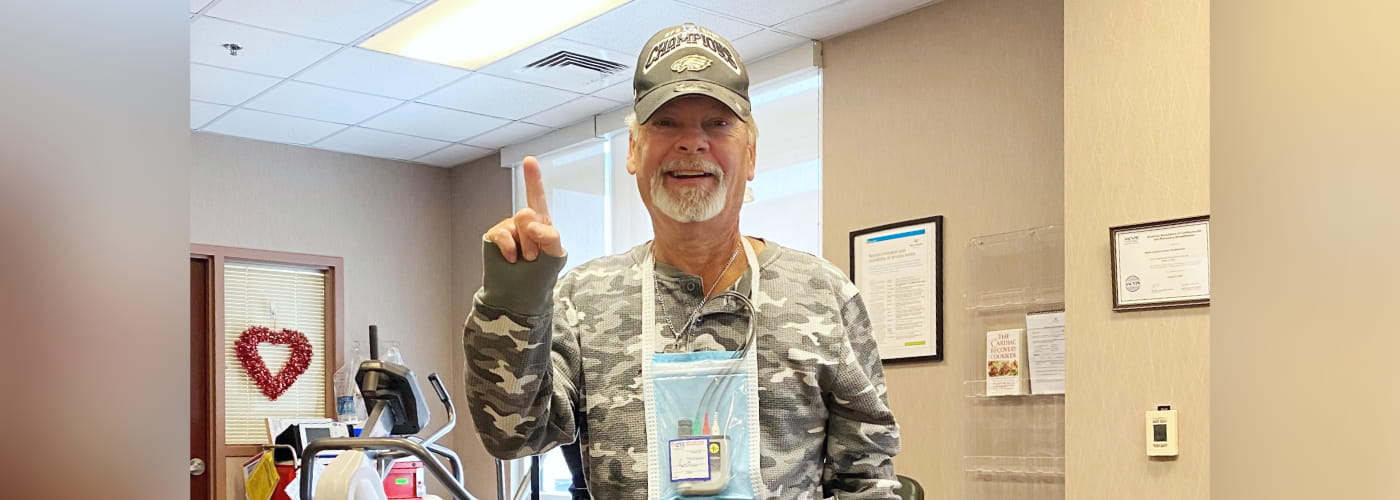
Surviving the widowmaker: How Radford came back healthier than before
On May 7, 2024, 68-year-old Radford Neary suffered a heart attack and cardiac arrest. For a moment, his heart stopped. What happened next is a story of survival, timing and how mere seconds made all the difference.