Before Surgery
Spine surgery pre-op checklist
- Choose a coach. Select a family member or friend who can drive you to the hospital on the day of surgery, pick up your prescriptions, drive you home on the day of discharge and drive you to medical appointments during recovery.
- Be prepared. For those who have a power of attorney or living will document for medical affairs and decisions, a copy of the document is required for your chart.
- Plan ahead. To make the days following surgery easier, review your home's arrangements to facilitate your recovery.
- Attend preadmission testing/clearances. Follow your surgeon's instructions for preadmission testing and medical clearance, which includes a physical examination, medical history and lab tests.
- Take preoperative shower(s). Follow the special bathing instructions in the preoperative shower section.
What to expect

- Surgery will last approximately two to four hours.
- You will be in the hospital approximately one night, as per your surgeon and insurance.
- You will generally go home the next day.
Post cervical laminectomy or fusion
- Surgery will last approximately four to six hours.
- You will be in the hospital one to two nights, as per your surgeon, your procedure and your insurance.
Lumbar discectomy
- Surgery will last approximately one hour.
- In most cases, you will go home the same day as surgery. If you are required to stay in the hospital, you will stay approximately one night, as per your surgeon, your procedure and your insurance.
Lumbar laminectomy
- Surgery will last approximately one to two hours.
- You will be in the hospital approximately one to two nights, as per your surgeon, your procedure and your insurance.
Lumbar fusion
- Surgery will last approximately two to three hours.
- You will be in the hospital approximately one to two nights,as per your surgeon, your procedure and your insurance.
Pre-op arrangements
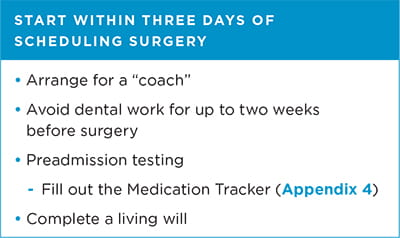
Arrange for a "coach"
Coaches are relatives or friends who:
- Help you prepare for surgery
- Assist with your recovery and rehabilitation
- Drive you to the hospital for your procedure and back home after discharge
- Pick up your outpatient pharmacy medications
Your coach will also be a first contact for updates from the health care team after surgery.
Manage your medical health
Speak with your primary care doctor about staying healthy for surgery, especially if you smoke, have diabetes or are obese.
Working with your physician to optimize your health reduces the risk of infections and poor wound healing.
If you are a current smoker, we advise you to:
- Quit smoking and/or using tobacco or nicotine products for at least two weeks BEFORE surgery.
- Avoid smoking cessation products such as Nicorette® gum, nicotine patches, nicotine vaping, and second-hand smoke. Nicotine, in any form, can delay bone fusion and healing.
Please discuss smoking cessation plans with your medical doctor. There are new medications available to help with this. Also, you may use the Main Line Health Contact Center at 1.866.CALL.MLH (225.5654) to find out about other resources or cessation classes.
Dental work
Two weeks before surgery
- Avoid extractions and periodontal work.
- If you require this work, please schedule well in advance of surgery.
The first 60 days after surgery
Do not schedule dental work—including routine cleanings.
More than 60 days after surgery
- Take one dose of antibiotic before receiving any dental care, if your surgeon recommends.
- Your surgeon will provide additional instructions during follow-up visit.
Preadmission testing and nursing assessment
- Health history and physical exam
- Blood work, EKG or X-rays
- Other medical appointments
Please have the following information filled out on the Medication Tracker (see Appendix 4*):
- Allergies and side effects from medications and anesthesia
- Medications (prescription and over-the-counter)
- Dose of each medication in milligrams (mg), milliliters (mL) or units, and when you take the medications (am vs. pm)
Please provide us with a list of dietary restrictions (e.g., vegetarian, gluten-free, kosher).
Finally, please plan to stay about two hours for pre-op clearance at the hospital or your physician's office.
- Your providers will give you instructions and go through your medication list.
- Your providers will also let you know what medication you can take the morning of surgery, if any are allowed.
Legal arrangements
If you have a power of attorney for medical affairs or a living will, you must provide copies of these documents in advance.
Insurance and copay information
For assistance from a financial counselor, see Appendix 1*.
Plan for surgery and recovery
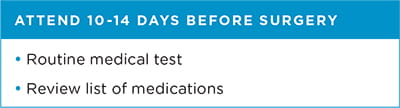
Seven to 14 days prior to surgery

Please note that for pain, you can take Tylenol as well as any other medications specifically approved by your surgeon.
If you take blood thinners (e.g., Plavix, Arixtra, Coumadin, Pradaxa, Eliquis or Xarelto), speak with the prescribing physician before stopping any of these medications.
In addition to being discontinued before surgery, some medications may not be resumed for up to 12 weeks after surgery to allow for bone healing. Please check with your surgeon for details on which medications need to be stopped and when your medications can be safely started again.
If you are asked to stop taking medications, please do so 10 to 14 days before surgery or as instructed.
If your surgeon indicates that you need to discontinue taking nonsteroidal anti-inflammatory drugs (NSAID), some of these drugs include the following:
- Ibuprofen (Advil/ Motrin)
- Naproxen (Aleve/Naprosyn)
- Meloxicam (Mobic)
- Celebrex
- Indocin
- Voltaren
- Lodine
You may also be asked to stop taking:
- Aspirin
- Osteoporosis medications (like Fosamax, Actonel)
- Vitamins, especially vitamin E and K and fish oil
- Over-the-counter supplements
- Hormone-related medications
Plan for at-home care after surgery
Ask yourself: While I'm recovering, who will help;
- Help me prepare meals?
- Take me home from the hospital, to my doctor appointments, and to physical therapy?
- Have my prescriptions filled upon discharge?
- Care for my pet while I'm in the hospital?
Important: Always wash hands well after contact with pets. Keep pets clean. No sleeping with pets after surgery.
Modify your home
Consider obtaining or placing:
- Firmly attached bars/handrails in shower/bath
- Stable chair with firm cushion and arm rests
- Raised toilet seat (your care manager can help)
- Items used daily within arm's reach for when you are home after surgery
- Throw rugs away from walking areas, prevent tripping over them during recovery
- Handheld items and aids you may need (per therapist 's advise during recovery)
Prior to discharge from the hospital, your therapists will advise you on what home modifications and aids you may need during your recovery.
Finally, complete your brace fitting (if one is required after surgery) BEFORE surgery and remember to pack your brace and bring it to the hospital the morning of surgery.
Note: Not all insurers pay for assistive devices.
- Discuss your PT needs with your surgeon.
- If you need outpatient therapy, choose a PT location that's close to home.
- Call your insurance company for therapy coverage and copay information.
- Plan for transportation to PT until you're cleared to drive.
The day before surgery
The day before your surgery, someone will call you between 2:00 pm and 5:00 pm with the scheduled time of your surgery and any additional details you might need.
Note: If your surgery is on Monday, you will be called on Friday afternoon.
Evening(s) before surgery
- Use the pre-op soap as directed by your surgeon (the next section reviews instructions on how to use this soap).
- Please refer to Anesthesia directions for fasting guidelines prior to surgery.
Plan on bringing to the hospital (if applicable to you):
- Photo identification, insurance cards and copay
- Glasses with a case, hearing aids and CPAP or BiPAP machine with mask (write down settings)
- Power of attorney documentation (if applicable)
- Your favorite personal hygiene products
- Shoes with good heel (sneakers, loafers)
- Loose-fitting pants (sweat pants, shorts) to accommodate dressings/bandages
- Patients can often become confused after surgery; pictures of loved ones can help you avoid this, as can crossword puzzles or a book
- Cell phone (with charger labeled with your name)
- Your brace if fitted for one before surgery
Plan on leaving the following at home
- Tight-fitting clothes and flip-flops (safety hazard)
- Jewelry, credit cards, valuables, large sums of cash
- Medications, unless told otherwise
Taking showers just before surgery
To reduce germs and your risk of infection:
- Wash hands frequently and clean skin daily.
- Follow your doctor's instructions on bathing, and on keeping dressings dry if you have any.
To prepare for surgery, wash with a special antiseptic soap, such as Hibiclens or Bactoshield. Available at local pharmacies (if not given by your surgeon's office or by Pre-Admission Testing), these soaps contain 4% chlorhexidine gluconate. If you're allergic to this or any other ingredients listed on the bottle, do NOT use these products. Talk to your provider about alternatives.
If you have tested positive for staph (staphylococcus/MRSA), follow the additional instructions in Appendix 7* regarding the preoperative skin cleansing schedule.
One or two nights before and the morning of surgery, shower or bathe with Bactoshield, Hibiclens or an alternative per surgeon request.
- Genital area
- Face
- Hair
For all other areas, Hibiclens or Bactoshield should replace your regular soap. Use this product as a liquid soap, applying directly to the skin and washing gently. Do not rub or scrub skin. Rinse thoroughly with warm water.
Do not use Hibiclens or Bactoshield in:
- Head, face, ears or mouth
- Genital area
After washing with antiseptic soap, do not:
- Wash with your regular soap
- Apply lotions, powders or perfumes to areas cleaned with the antiseptic soap
- Use hair removal products or shave at or near the surgical site 48 hours before your procedure
Do not use hair removal products or shave at or near the surgical site within 48 hours before your procedure.
To schedule an appointment with an spine specialist at Main Line Health, call 1.866.CALL.MLH (225.5654) or use our secure online appointment request form.
*Every appendix referenced throughout this content can be found in the print version of your guide to preparing for spine surgery (PDF).