Telemedicine provides LGBTQ care for patients in isolation

For weeks we’ve been hearing words such as “elective” and “essential,” often weighing in our minds whether one thing is as important as another during the coronavirus outbreak. In health care, surgeries have been canceled and some physician offices have had limited or no in-person hours at all. For some LGBTQ patients, whether someone who’s just coming out, or a transgender person who is already receiving gender-affirming hormones, this disruption in regular care can have frightening and unnecessary consequences.
College students may be home without the usual supports offered at colleges and community events. Not having regular face-to-face dating encounters can also be particularly isolating, according to Dane Menkin, CRNP, nurse practitioner with Bryn Mawr Family Practice and director of LGBTQ services at Main Line Health. Transgender people who may have begun treatment have a real need for timely continuation of care.
Thanks to telemedicine—rapidly rolled out and widely adopted within weeks of the Pennsylvania statewide COVID-19 stay-at-home order—LGBTQ care is now available right in their own homes. And it is this touchpoint with primary care providers by video that Menkin says is allowing physical check-ins, such as STD consults or demonstration of self-injection of gender-affirming hormones, as well as the mental health support that many LGBTQ patients need but cannot get elsewhere.

COVID-19 stay-at-home order—LGBTQ care is now available right in their own homes.
“It is the example of how you can reach a population that often has unmet needs and do a lot of good,” Menkin adds. “Just talking with another person openly is validating and affirming and relieves isolation, which then can alleviate depression.”
LGBTQ mental and physical health risks
Many studies show higher rates of depression among LGBTQ people, a segment of the population that is less inclined to seek medical care in general, partly due to past negative experiences in health care settings.
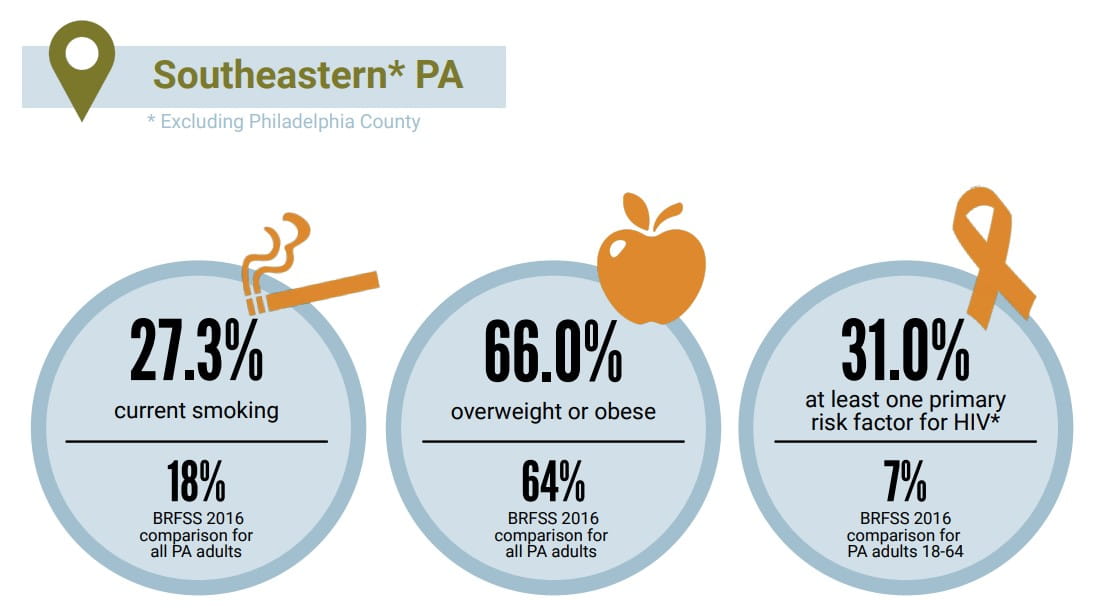
LGBTQ individuals are also more likely to use tobacco, more likely to have problems with substance use, and more likely to have risk factors for HIV. A 2018 LGBT health needs assessment for southeastern Pennsylvania indicates poor health behaviors and factors compared to other Pennsylvania adults in several areas:
Without the usual barriers of transportation or concerns about the waiting room, telemedicine makes LGBTQ care more readily available to more people, more quickly and more often—and Menkin hopes to see this favorable trend continue beyond COVID-19. Gaining access to highly competent and compassionate care is seen as a privilege in many places. Telehealth makes care accessible to LGBTQ people everywhere.
Menkin further emphasizes the importance of consulting with a doctor if you’re concerned about having had an encounter and being exposed to HIV or a sexually transmitted disease (STD). “Talk to us on the phone and we’ll assess the risk/benefit of going to the lab and having blood work done.” Labs are still open in spite of COVID-19 but they’re not accepting walk-ins or patients without an appointment, so you’ll need to call your provider first.
“If you are taking PrEP (Pre-exposure Prophylaxis) to prevent HIV transmission and are wondering whether to continue taking your medications during this time when many are less sexually active, be sure to check with your clinician,” Menkin advises. “Keep in mind, although there are some small studies looking at their use for treatment, the medicines used for PrEP do not prevent you from you from getting COVID.”
People living with HIV have not been identified as being at an increased risk for COVID by the Centers for Disease Control. The World Health Organization also states in an extensive FAQ about COVID-19, HIV and antiretrovirals: “At present there is no evidence that the risk of infection or complications of COVID-19 is different among people living with HIV who are clinically and immunologically stable on antiretroviral treatment when compared with the general population.”
Meanwhile, adds Menkin, “Life moves on. The pharmacies are open, patients can get medicines. We want people to know that whether you’re a new or established patient, we’re providing telehealth LGBTQ care and continuation of care to all the vulnerable patients we see.”
To schedule an appointment with a Main Line Health LGBTQ Inclusive Care specialist, please call the confidential telephone line at 484.337.LGBT (5428) or email us at lgbtq@mlhs.org.
Main Line Health serves patients at hospitals and health centers throughout the western suburbs of Philadelphia. To schedule an appointment with a specialist at Main Line Health, call 1.866.CALL.MLH (225.5654).
 Content you want, delivered to your inbox
Content you want, delivered to your inbox
Want to get the latest health and wellness articles delivered right to your inbox?
Subscribe to the Well Ahead Newsletter.
