Preparing for Joint Replacement Surgery
Pre-op arrangements
When preparing for your joint replacement surgery, there are a number of things you will need to do to help make your surgery and recovery as successful as possible.
Soon after scheduling surgery
- Register for pre-op education
- Arrange for a "coach"
- Complete a living will
- Avoid dental work for up to two weeks before surgery
- Preadmission testing
- Fill out Medication Tracker (Appendix 3)
Arrange for a “coach”
During the weeks before your surgery, many people will be asking you about your insurance coverage, medical history, legal arrangements and support plan for when you get home. The following may help:
- Arrange for a "coach"—this is a family member or friend who will be taught how to assist you with planning and recovery. This person will act as the first person to receive information from your doctor and health care team.
- If you have a power of attorney for medical affairs or a living will that indicates your health care decisions, you must provide copies of these documents in advance.
Manage your medical health
peak with your primary care doctor about staying healthy for surgery, especially if you smoke, have diabetes or are obese.
Working with your physician to optimize your health reduces the risk of infections and poor wound healing.
If you are a current smoker, we advise you to:
- Quit smoking and/or using tobacco or nicotine products for at least two weeks BEFORE surgery.
- Avoid smoking cessation products such as Nicorette® gum, nicotine patches, nicotine vaping, and second-hand smoke. Nicotine, in any form, can delay healing.
Please discuss smoking cessation plans with your doctor. There are new medications available to help with this. Also, you may use the Main Line Health Contact Center at 1.866.CALL.MLH (225.5654) to find out about other resources or cessation classes.
Dental work
Two weeks before surgery
- Avoid extractions and periodontal work.
- If you require this work, please schedule well in advance of surgery.
The first 90 days after surgery
DO NOT schedule any invasive procedures including dental work or dental cleaning.
More than 90 days after surgery
- Take one dose of antibiotic before receiving any dental care, if your surgeon recommends.
- Your surgeon will provide additional instructions during follow-up visit.
Preadmission testing and nursing assessment
Attend 10-14 days before surgery
- Routine medical test
- Review list of medications
Your surgeon will provide instructions on medical evaluations needed before surgery, such as:
- Health history and physical exam
- Blood work, EKG or X-rays
- Other medical clearances
Please have the following information filled out on the Medication Tracker (see Appendix 3 of the PDF guide):
- Allergies and side effects from medications and anesthesia
- Medications (prescription and over-the-counter)
- Dose of each medication in milligrams (mg), milliliters (mL) or units, and when you take the medications (AM vs. PM)
Please provide us with a list of dietary restrictions (e.g., vegetarian, gluten-free, Kosher).
Finally, please plan to stay about two hours for preop clearance at the hospital or your physician's office.
- Your providers will give you instructions and go through your medication list.
- Your providers will also let you know what medication you can take the morning of surgery, if any are allowed.
Insurance and copay information
For assistance from a financial counselor, please call pre-surgery billing/financial counseling for all hospitals at 484.337.1970.
Plan for surgery and recovery
Seven to 14 days prior to surgery
Follow your surgeon's instructions on discontinuing medications during this time. Those instructions may be in your surgeon's pre-op check list; please refer to that list if you received one.
Please note that for pain, you can take Tylenol as well as any other medications specifically approved by your surgeon.
If you take blood thinners (e.g., Plavix, Arixtra, Coumadin, Pradaxa, Eliquis or Xarelto), speak with the prescribing physician before stopping any of these medications.
In addition to being discontinued before surgery, some medications may not be resumed for up to 12 weeks after surgery to allow for bone healing. Please check with your surgeon for details on which medications need to be stopped and when your medications can be safely started again.
If you are asked to stop taking medications, please do so 10 to 14 days before surgery or as instructed.
If your surgeon indicates that you need to discontinue taking nonsteroidal anti-inflammatory drugs (NSAID), some of these drugs include the following:
- Ibuprofen (Advil/Motrin)
- Naproxen (Aleve/Naprosyn)
- Meloxicam (Mobic)
- Celebrex
- Indocin
- Voltaren
- Lodine
You may also be asked to stop taking:
- Aspirin
- Osteoporosis medications (like Fosamax, Actonel)
- Vitamins, especially vitamin E and K and fish oil
- Over-the-counter supplements
- Hormone-related medications
Plan for at-home care after surgery
Ask yourself: While I'm recovering, who will…
- Help me prepare meals?
- Take me home from the hospital, to my doctor appointments, and to physical therapy as directed by my surgeon?
- Have my prescriptions filled upon discharge?
- Care for my pet while I'm in the hospital?
IMPORTANT: Always wash hands well after contact with pets. Keep pets clean. No sleeping with pets after surgery.
Quick Tip
- Frequent hand washing and daily skin cleansing promotes good health and hygiene. Daily skin cleansing helps remove microbes (germs) that may cause infections. This is especially important if you are having a surgical procedure.
Pre-op exercises
Pre-surgery exercise is an important part of the joint replacement journey. Follow your surgeon's plan and take part in pre-op physical therapy, if recommended.
Remember to breathe:
- Inhale just before you start the exercise.
- Exhale while you perform the exercise.
- Do not hold your breath. Count aloud when performing holding (isometric) exercises.
The five exercises below are the most important to do consistently up to the day before surgery. Repeat each exercise one to two times per day on BOTH legs. If there is any one exercise that hurts, skip it.
You will perform each of the leg and ankle exercises while lying down on a flat surface, such as a couch or bed, with your legs out straight.
1. Gluteal sets

- Squeeze buttocks together.
- Hold for 10 seconds, remembering to breathe.
- Relax your buttocks.
- Repeat 10 to 20 times.
2. Hamstring sets
- Dig your left heel into the bed or couch. By doing so, you will feel the muscle on the back of your thigh tighten.
- Hold for 10 seconds, remembering to breathe.
- Relax your leg.
- Repeat 10 to 20 times.
- Repeat exercise with other leg.
3. Quad sets
- Press the back of one of your knees down into the bed or couch. By doing so, you will feel the muscle on the front of your thigh tighten.
- Hold for 10 seconds, remembering to breathe.
- Relax your leg.
- Repeat 10 to 20 times.
- Repeat exercise with other leg.
4. Ankle pumps
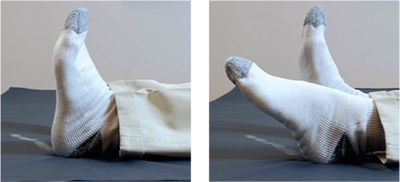
- Point toes toward ceiling.
- Bend your ankles up and down, as if you were pumping a gas pedal. You may do this with both feet together or alternating feet.
- Repeat 20 times.
5. Strengthening your arms
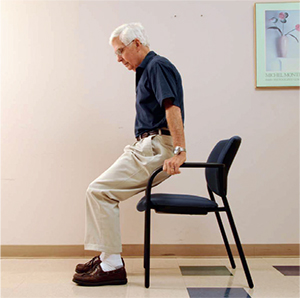
This exercise helps strengthen your arms for walking with crutches or a walker. It makes getting out of a chair easier and is especially helpful for patients who are having bilateral (both) knee or hip replacements.
For this exercise you will start from a seated position in an arm chair.
- Sit with your knees bent and feet flat on the floor.
- Place hands on armrests.
- Straighten arms by pushing down and raising your bottom up off the chair (if possible).
- Hold for five seconds.
- Slowly lower yourself back into the chair.
- Repeat 10 to 20 times.
Modify your home
Consider obtaining or placing:
- Firmly attached bars/handrails in shower/bath
- Stable chair with firm cushion and armrests
- Raised toilet seat
- Items used daily within arm's reach for when you are home after surgery
- Throw rugs away from walking areas, prevent tripping over them during recovery
- Handheld items and aids you may need (per therapist's advice during recovery)
Prior to discharge from the hospital, your therapists will advise you on what home modifications and aids you may need during your recovery.
Note: Not all insurers pay for assistive devices.
Physical therapy (PT) once you're home: How to plan ahead of time
If physical therapy will be part of your recovery plan, it is your responsibility to make appointments and coordinate rides to appointments until you have been cleared to drive by your surgeon. If physical therapy is part of your postsurgery plan, be sure to contact your insurance company in advance to find out about outpatient physical therapy coverage and copay information.
Equipment
The items you may need following surgery include:
- Walker with front wheels only, no brakes or seat (this can be provided for your hospital stay and may be given to you as you are discharged—insurance approval for coverage not guaranteed)
- Cane
Other handheld items you may need and may be available for purchase in the hospital gift shop include:
- Grabber Reacher
- Long-handled shoe horn
- Dressing stick
Note: Not covered by insurance.
The day before surgery
The day before your surgery, someone will call you between 2:00–5:00 pm with the scheduled time of your surgery and provide any additional details you might need.
Note: If your surgery is on Monday, you will be called on Friday afternoon.
Evening(s) before surgery
- Use the pre-op soap as directed by your surgeon (the next section reviews instructions on how to use this soap).
- Please refer to anesthesia directions for fasting guidelines prior to surgery.
Plan on bringing to the hospital (if applicable to you)
- Photo identification, insurance cards and copay
- Glasses with a case, hearing aids and CPAP or BiPAP machine with mask (write down settings)
- Power of attorney documentation (if applicable)
- Your favorite personal hygiene products
- Shoes with good heel (sneakers, loafers)
- Loose-fitting pants (loungewear or shorts) to accommodate dressings/bandages
- Patients can become temporarily confused after surgery; pictures of loved ones can help you avoid this, as can crossword puzzles or a book
- Cell phone (with charger labeled with your name)
- Walkers (bring for sizing purposes only, if your walker was not purchased and sized for you)
Quick tip
To access your lab work or care summary after discharge, sign up for Main Line Health MyChart before surgery.
Plan on leaving the following at home
- Tight-fitting clothes and flip-flops (safety hazard)
- Jewelry, credit cards, valuables, large sums of cash
- Medications, unless told otherwise
Taking showers just before surgery
One or two nights before surgery and the morning of surgery
- Read instructions provided by your health care provider.
- Use Bactoshield or Hibiclens soaps, unless allergic to these soaps.
- If allergic to these soaps, use an alternative recommended by your physician.
To reduce germs and your risk of infection:
- Wash hands frequently and clean skin daily.
- Follow your doctor's instructions on bathing, and on keeping dressings dry if you have any after surgery.
To prepare for surgery, wash with a special antiseptic soap, such as Hibiclens or Bactoshield. Available at local pharmacies (if not given by your surgeon's office or by Pre-Admission Testing), these soaps contain 4% chlorhexidine gluconate. If you're allergic to this or any other ingredients listed on the bottle, do NOT use these products. Talk to your provider about alternatives.
If you are positive for staph (staphylococcus/MRSA), follow the additional instructions in Appendix 6 of the PDF guide regarding the preoperative skin cleansing schedule.
One or two nights before and the morning of surgery, shower or bathe with Bactoshield, Hibiclens or an alternative per surgeon request.
Use regular soap and shampoo for the following areas, rinsing thoroughly to remove residue:
- Genital area
- Face
- Hair
For all other areas, Hibiclens or Bactoshield should replace your regular soap. Use this product as a liquid soap, applying directly to the skin and washing gently. Do not rub or scrub skin. Rinse thoroughly with warm water.
Do not use Hibiclens or Bactoshield in:
- Head, face, ears or mouth
- Genital area
After washing with antiseptic soap, do not:
- Wash with your regular soap
- Apply lotions, powders or perfumes to areas cleaned with the antiseptic soap
- Use hair removal products or shave at or near the surgical site 48 hours before your procedure
DO NOT USE HAIR REMOVAL PRODUCTS OR SHAVE AT OR NEAR THE SURGICAL SITE WITHIN 48 HOURS BEFORE YOUR PROCEDURE.